"Fentanyl Exposure" in 8 Charts
I teamed up with the Center for Just Journalism to analyze how the media covers so-called "fentanyl exposure" incidents among police officers.
A lot of heavy lifting over the course of a year and I can finally say this week that a huge project has gone live: Fentanyl Exposure: Myths, Misconceptions, and The Media, a report featuring original research—by yours truly—into the scope of outlandish coverage of fentanyl exposure among police, published by the nonprofit Center for Just Journalism.
For those of you who have followed my reporting on this issue, these results will not be much of a surprise. Still, there is quite a bit of novelty and originality in this report. In particular, this is probably the most detailed, granular, and sweeping account of just how wrong news outlets got this story.
I’ll briefly go over how the analysis was done and then share the highlights.
Basically, this is a content analysis. Scholars in media, communications, and lots of other disciplines frequently do these kinds of big studies. Using LexisNexis and a bespoke keyword code, I searched for news stories about opioid exposure published in English language news outlets between January 2018 and May 2023. That search turned up about 1,100 articles. Then, I divided up the articles to be coded by myself and a team. If an article was deemed relevant, meaning it was covering “fentanyl exposure” in anyway, then we applied an original codebook to glean as much information as possible about how the news article covered the topic.
We recorded information about the news outlet itself (was it local, national, etc.), then we wanted details of the incident, sources quoted, any attempts to verify the claims made by sources, and whether the article expressed doubt about the incident. Were any doctors or scientists quoted? Was the vast literature debunking the phenomenon even referenced? Were the basics of journalistic due diligence applied?
The answer, overwhelmingly, is no. From 2018 to 2023, the news media utterly failed to get this story right.
Fentanyl Exposure in 8 Charts
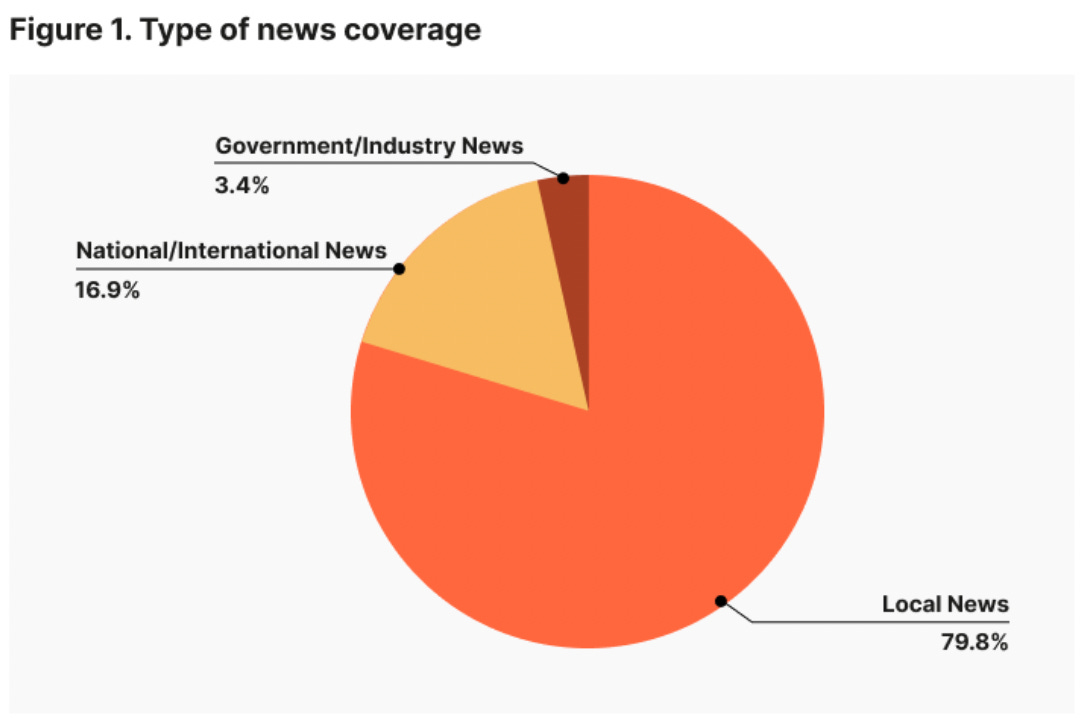
#1. Roughly eighty percent of the news articles covering fentanyl exposure incidents ran in the local news.
#2. Out of 326 news articles mentioning fentanyl exposure, 252 quoted police sources while just 35 quoted medical experts.
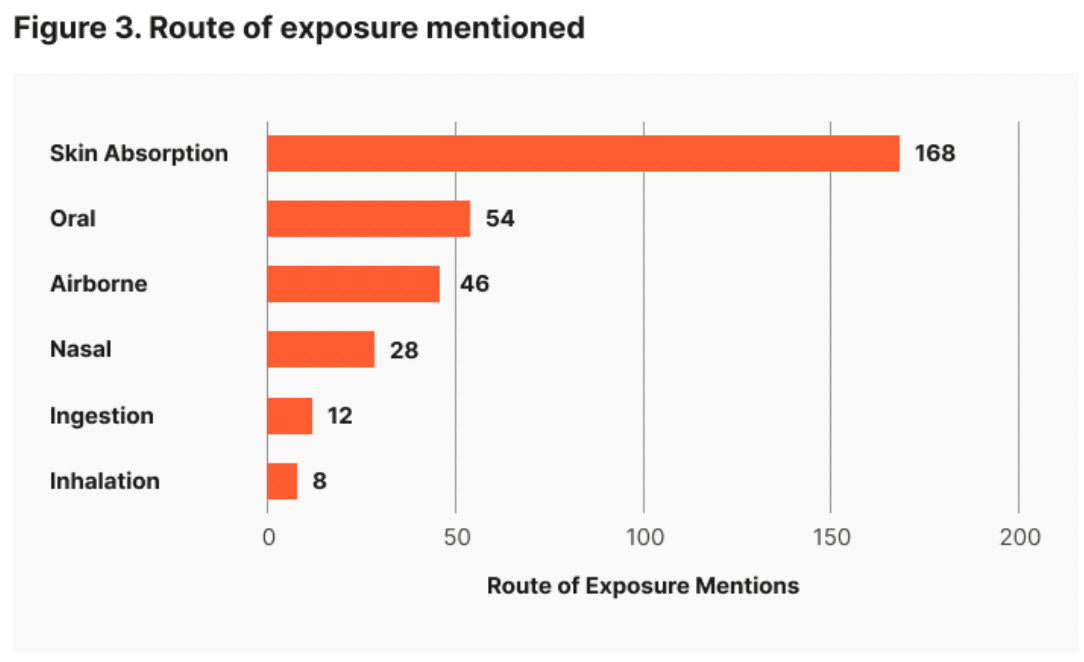
#3 The most commonly named route of exposure was skin contact, which, out of all exposure routes, is the least plausible to cause any toxic effect.
Skin exposure always requires some explaining. To have a clinical effect, opioids must enter the body and reach the bloodstream, cross the blood-brain barrier, where the molecules attach to certain receptors. (Drug users know this, which is why fentanyl is used by injecting, snorting, or smoking.) Fentanyl does not travel through skin easily, quickly, or in large enough doses. Transdermal fentanyl patches do exist for chronic pain. Still, a concentrated dose of fentanyl delivered through skin requires constant contact over a long period of time.
These facts contradict accounts by police who say they overdosed after “touching” the drug. A small dusting of fentanyl on your skin simply cannot produce an overdose. That is impossible. Although fentanyl can be absorbed by breathing into the lungs or by contacting the mucous membranes in the nose, this is extremely unlikely because the drug must be made into an aerosolized form to go up into the air. Fentanyl particles—like the powder on the street—are heavier than the atmosphere. If Sir Isaac Newton is correct that a thing called gravity exists, then these particles will not linger in the air. They will fall quickly fall to the ground.
Lastly, in case you weren’t yet convinced, you also have to consider drug purity. Illicitly manufactured fentanyl tends to be highly impure. It is cut with all kinds of benign or not-so-benign cutting agents and fillers. The DEA puts purity average at a range of just 1 to 10 percent. Accidental exposure to a clinically significant dose is even more unlikely given the very small amount of actual fentanyl in the pills and powders that police might encounter. I once spoke to a doctor named Ryan Feldman who spilled a shit load of pure liquid fentanyl. He didn’t panic. He didn’t overdose. He just went to a sink and washed it off without incident. That was pure, pharma-grade fentanyl and nothing happened. He was fine.
Moving on….
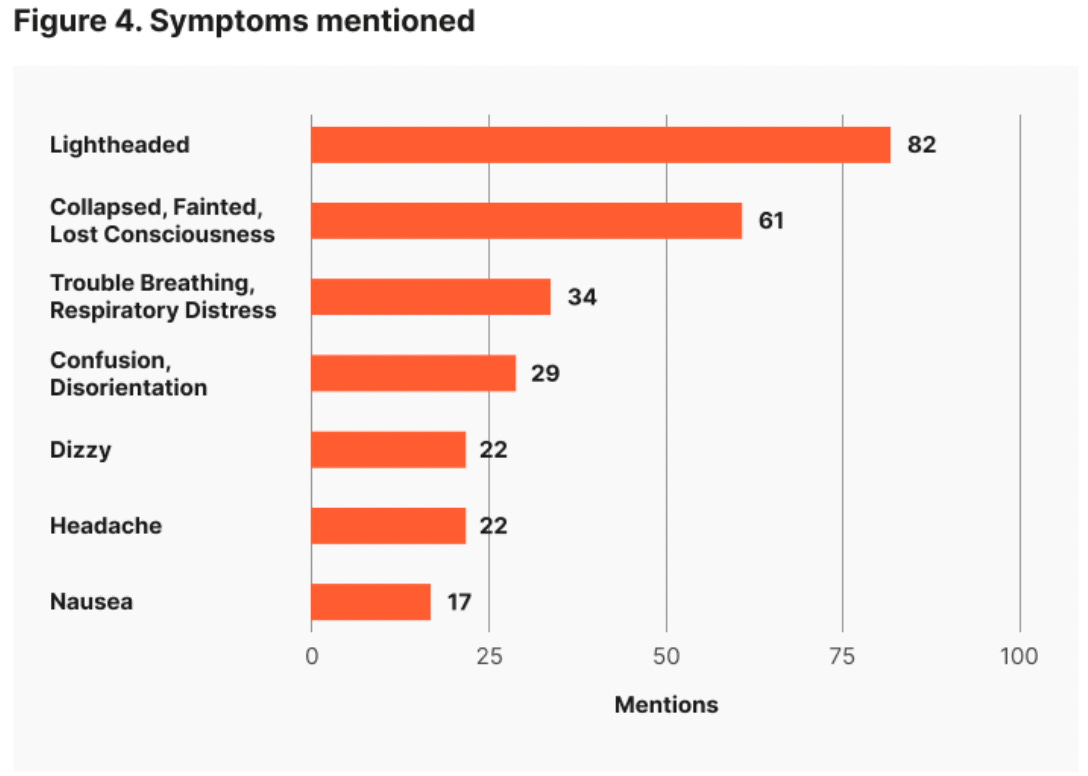
#4. The most common symptom mentioned was lightheadedness (82 articles) followed by collapsing, fainting, or loss of consciousness. These are not really symptoms of opioids.
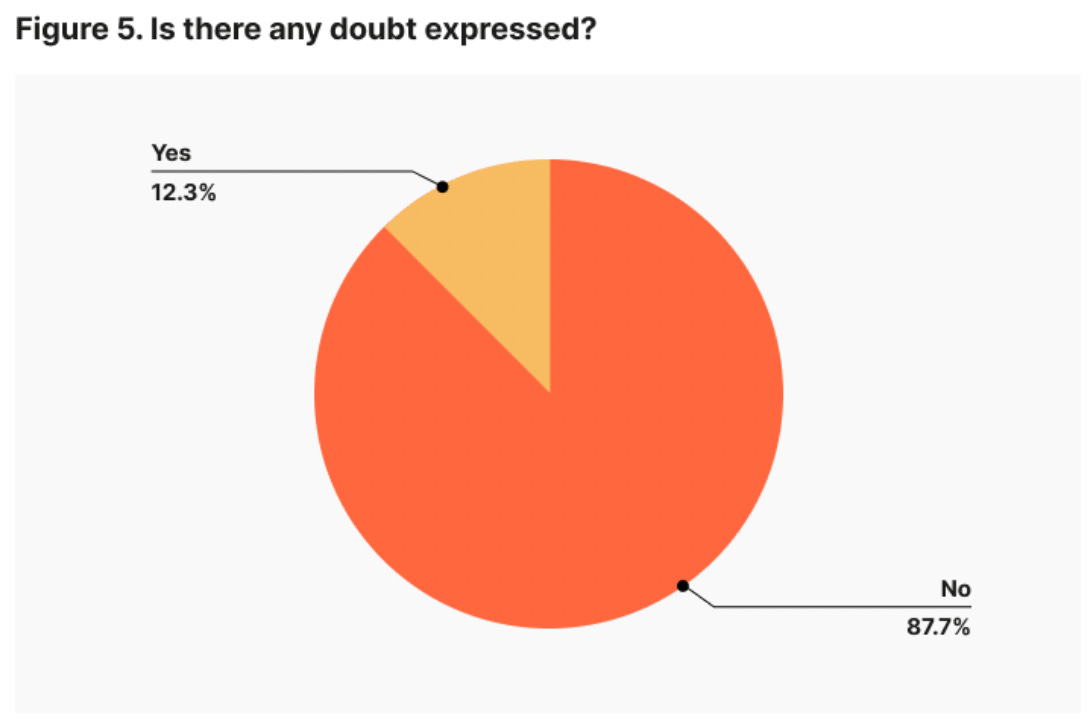
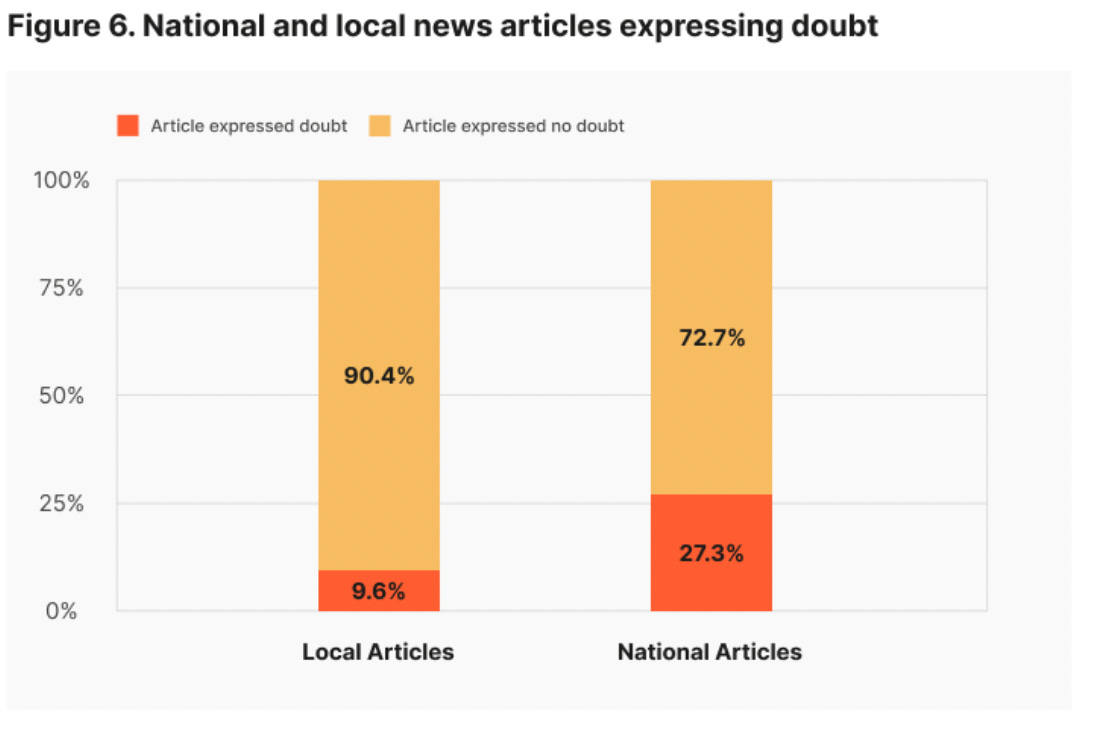
#5. Just 40 articles (12 percent) included an expression of doubt about the danger of passive fentanyl exposure, while 286 articles (87 percent) expressed no doubt.
#6. National news outlets were more likely to express skepticism about purported exposure incidents than local news outlets.
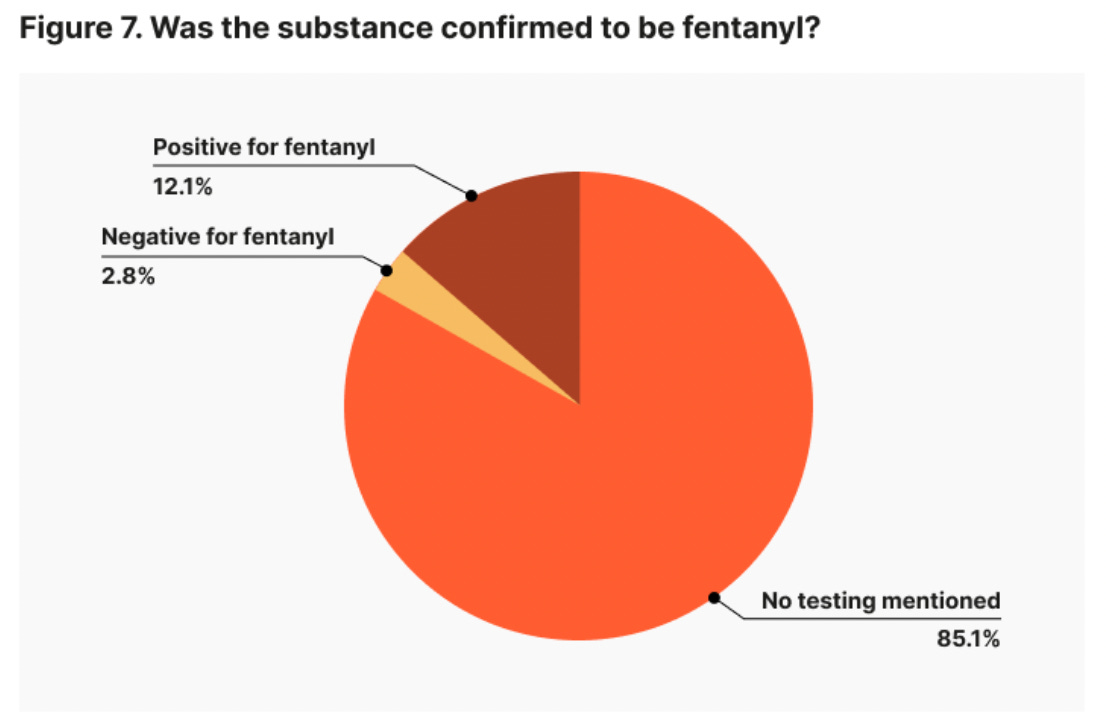
#7. Only 12 percent of articles reported that the substance was confirmed to be fentanyl, while 85 percent made no mention that the substance was tested and confirmed using validated techniques.
And finally…..
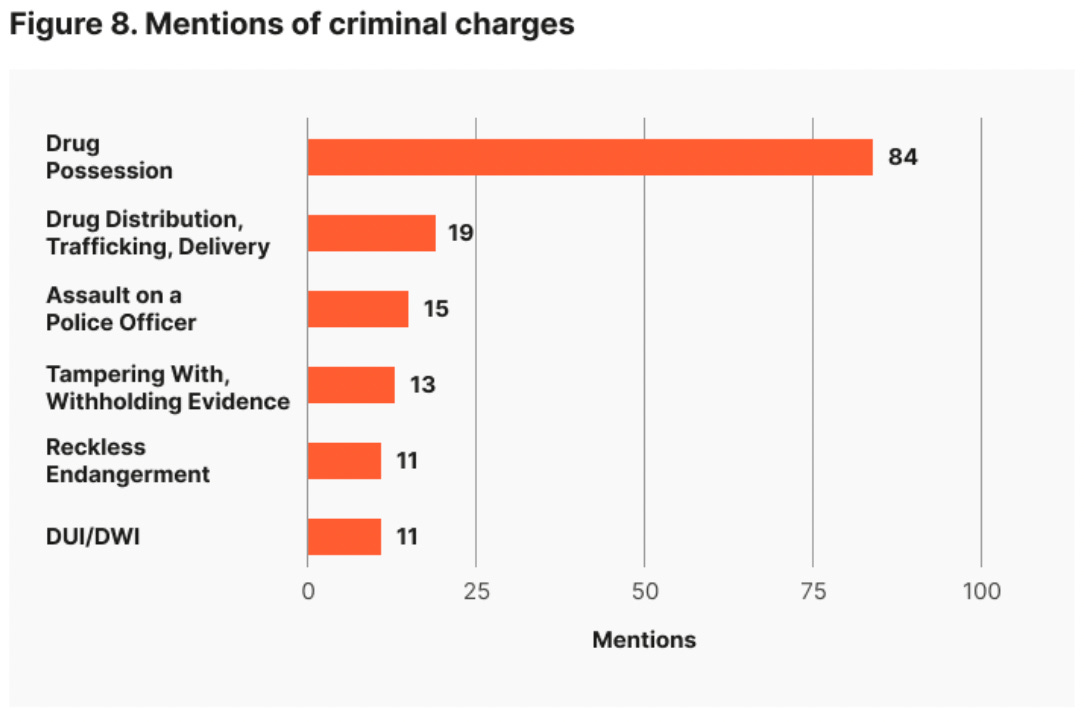
#8. Arrests and criminal charges were mentioned in 155 (47%) of articles. Although drug possession was the most commonly named charge, other articles mentioned assault on a police officer and/or reckless endangerment charges.
To summarize this up… the results are not good.
Key Findings:
The vast majority of news articles failed to cite the large and growing body of scientific literature proving that incidental exposure to fentanyl is not dangerous.
The vast majority of news articles exclusively relied on police sources and neglected to quote medical experts.
Not a single news article presented physical evidence, such as toxicological testing, confirming that the symptoms were caused by fentanyl.
Suspects accused of causing exposure are being charged with assaulting a police officer, and states are passing new laws that criminalize those alleged to have caused exposure.
Thanks for checking this out. It was a lot of hard and quite tedious work to pull off but I’m glad we did it. I’m massively grateful to Laura Bennett from the Center for Just Journalism, and her right-hand Hannah Riley. They crushed it.
I’m also indebted to Dr. Andrew Stolbach, of Johns Hopkins, who helped me conceptualize the structure of the analysis. And Bella Horton, for helping create the codebook and for the many hours of coding.
If you think this kind of work is of value, then please subscribe to this newsletter so I can keep it going. Thank you. - Zach



Touching Fentanyl has no effect on you. I have never used Fentanyl but have touched it multiple times. It’s total BS that by touching Fentanyl it does anything to you.